What is a Cervical Spondylosis?
Cervical spondylosis is a condition that affects the neck region of the spine. It is characterized by the degeneration of the bones, discs, and joints in the cervical spine, which is the upper part of the spine located in the neck. This degeneration is often a result of the natural aging process, although other factors such as injury, poor posture, and genetic predisposition can also contribute to its development.
As we age, the intervertebral discs in the cervical spine gradually lose moisture and become less flexible. They may develop small cracks or tears, leading to bulging or herniation. Additionally, the cartilage and bones in the neck can undergo degenerative changes, such as the formation of bone spurs or the development of osteoarthritis.
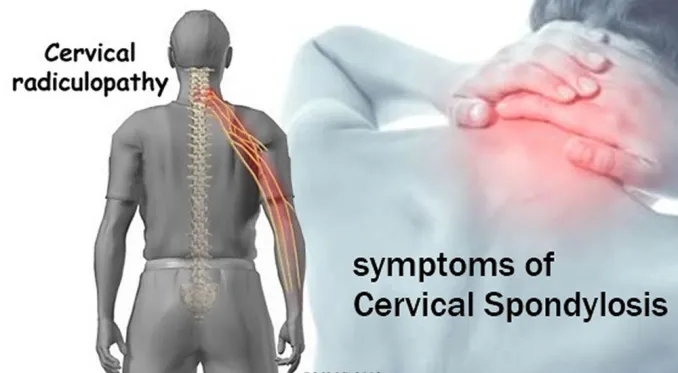
The symptoms of cervical spondylosis can vary from person to person. Common symptoms include neck pain and stiffness, which may radiate to the shoulders or arms. Some individuals may also experience headaches, numbness or tingling in the arms or hands, muscle weakness, and difficulty with coordination. In severe cases, cervical spondylosis can cause compression of the spinal cord or nerve roots, leading to more severe symptoms like loss of balance or bowel/bladder dysfunction.
Diagnosing cervical spondylosis typically involves a combination of medical history, physical examination, and imaging studies. X-rays, magnetic resonance imaging (MRI), or computed tomography (CT) scans can provide detailed images of the cervical spine, helping to identify any abnormalities.
The treatment of cervical spondylosis aims to alleviate pain, improve mobility, and prevent further damage. Conservative measures such as rest, physical therapy, pain medications, muscle relaxants, and the use of cervical collars or braces are often recommended. In some cases, corticosteroid injections may be used to reduce inflammation and pain. Surgery may be considered in severe cases or when conservative treatments do not provide adequate relief. Surgical options can involve decompressing the spinal cord or nerve roots, removing bone spurs, or stabilizing the spine.
While cervical spondylosis cannot be entirely prevented, certain lifestyle modifications can help manage the condition and reduce the risk of further damage. Maintaining good posture, avoiding excessive strain on the neck, regular exercise to strengthen the neck muscles, and avoiding activities that exacerbate symptoms can be beneficial.
If you suspect you may have cervical spondylosis or are experiencing neck pain and related symptoms, it is important to consult with a healthcare professional for an accurate diagnosis and appropriate management plan. They can provide personalized guidance and treatment options based on your specific condition.
Related Anatomy
To understand cervical spondylosis, it’s helpful to have a basic understanding of the related anatomy of the cervical spine. Here are some key anatomical structures involved:
- Cervical Spine: The cervical spine is the uppermost part of the vertebral column, consisting of seven vertebrae (C1-C7). These vertebrae provide support, flexibility, and protection to the spinal cord, nerves, and blood vessels within the neck region.
- Intervertebral Discs: Between each pair of cervical vertebrae, there is an intervertebral disc. These discs act as shock absorbers and allow for movement and flexibility in the neck. Each disc consists of an outer fibrous ring called the annulus fibrosus and a gel-like center called the nucleus pulposus.
- Vertebrae: The cervical vertebrae are numbered C1 to C7, starting from the top. The first two vertebrae have unique structures:
- C1 (Atlas): The atlas is the first cervical vertebra, supporting the skull and allowing for nodding motion. It lacks a vertebral body and instead consists of a ring-like structure with two lateral masses that articulate with the skull and C2.
- C2 (Axis): The axis is the second cervical vertebra and has a unique structure called the dens or odontoid process. The dens protrudes upward from the vertebral body and forms a pivot joint with the atlas, allowing for rotational movement of the head.
- Spinal Cord: The spinal cord is a long, cylindrical bundle of nerve tissue that extends from the brainstem to the lumbar region of the spine. It passes through the central canal within the vertebrae and is responsible for transmitting sensory and motor signals between the brain and the rest of the body.
- Nerve Roots: Between each pair of cervical vertebrae, spinal nerve roots exit the spinal cord through small openings called intervertebral foramina. These nerve roots then branch out to supply sensation and motor control to specific areas of the body.
- Joints: The cervical spine has various joints that facilitate movement and stability. These include:
- Facet Joints: Found on the posterior aspect of each vertebra, these joints connect adjacent vertebrae and allow for bending, twisting, and extension of the neck.
- Atlanto-occipital Joint: Located between the atlas (C1) and the base of the skull, this joint allows for nodding or flexion/extension movement of the head.
- Atlantoaxial Joint: Formed by the articulation between the atlas (C1) and the axis (C2), this joint permits rotational movement of the head.
Understanding the anatomy of the cervical spine can help in comprehending the structures involved in cervical spondylosis and how they may be affected by degenerative changes.
Causes of Cervical Spondylosis
The primary cause of cervical spondylosis is the natural aging process and the wear and tear that occurs on the cervical spine over time. However, there are several factors that can contribute to the development of cervical spondylosis. Here are some common causes:
- Aging: As we age, the structures of the spine naturally degenerate. The intervertebral discs lose moisture and elasticity, becoming thinner and less flexible. The vertebral bones may develop osteoarthritis, and the ligaments and muscles supporting the cervical spine may weaken.
- Wear and Tear: Repetitive stress and strain on the cervical spine due to poor posture, heavy lifting, or certain occupations that involve constant neck movements can accelerate the degenerative changes. This can include activities such as prolonged sitting with a forward head posture, repetitive bending or twisting of the neck, or activities that involve heavy lifting.
- Spinal Injuries: Previous injuries or trauma to the neck, such as whiplash from car accidents, falls, or sports-related injuries, can increase the risk of developing cervical spondylosis later in life. Injuries can cause damage to the discs, vertebrae, ligaments, or muscles, leading to accelerated degeneration.
- Genetic Factors: There may be a genetic predisposition to developing cervical spondylosis. Some individuals may inherit certain traits or characteristics that make them more susceptible to the degenerative changes in the cervical spine.
- Smoking: Smoking has been associated with an increased risk of developing cervical spondylosis. It is believed that smoking reduces blood flow to the spinal discs, depriving them of necessary nutrients and impairing their ability to heal or regenerate.
- Other Factors: Certain conditions such as rheumatoid arthritis, ankylosing spondylitis, or genetic disorders affecting the spine can contribute to the development of cervical spondylosis. These conditions can cause inflammation, joint abnormalities, or accelerated degeneration in the cervical spine.
It’s important to note that while these factors can contribute to the development of cervical spondylosis, the condition is primarily a result of the natural aging process. It is a common condition that affects a significant portion of the population, especially in older adults.
Symptoms of Cervical Spondylosis
Cervical spondylosis can cause a variety of symptoms that can vary from person to person. Some individuals may experience mild symptoms, while others may have more severe or debilitating ones. Here are the common symptoms associated with cervical spondylosis:
- Neck Pain: One of the most common symptoms is neck pain, which can range from mild to severe. The pain is often localized to the neck region but may radiate to the shoulders, upper back, or arms. It can be described as a dull ache, sharp pain, or a feeling of stiffness and tightness in the neck. Neck muscle spasm also associated.
- Stiffness and Limited Range of Motion: Cervical spondylosis can lead to stiffness in the neck, making it difficult to turn or move the head fully. The range of motion may become limited, and it may be challenging to perform activities that involve neck movements.
- Headaches: Some individuals with cervical spondylosis may experience headaches, particularly in the back of the head or at the base of the skull. These headaches can be caused by muscle tension, nerve compression, or referred pain from the cervical spine.
- Radiculopathy: When the nerves in the cervical spine become compressed or irritated, it can lead to radiculopathy. Radiculopathy refers to the pain, numbness, tingling, or weakness that radiates from the neck into the shoulders, arms, and hands. The specific areas affected depend on which nerve roots are involved.
- Muscle Weakness: In some cases, cervical spondylosis can cause muscle weakness in the arms or hands. This weakness may make it challenging to grip objects, perform fine motor tasks, or feel a loss of strength in the affected areas.
- Coordination and Balance Problems: If the spinal cord becomes compressed due to severe cervical spondylosis, it can lead to coordination and balance problems. This can manifest as difficulty with walking, unsteadiness, or a feeling of clumsiness.
- Numbness and Tingling: Compression or irritation of the nerves in the cervical spine can cause numbness and tingling sensations in the shoulders, arms, and hands. These sensations may be intermittent or constant, and they can affect one or both sides of the body.
- Loss of Bowel or Bladder Control (Rare): In severe cases of cervical spondylosis, where there is significant compression of the spinal cord, it is possible to experience loss of bowel or bladder control. This is a rare but serious symptom that requires immediate medical attention.
It’s important to note that not all individuals with cervical spondylosis will experience all of these symptoms. The severity and combination of symptoms can vary depending on the extent of degeneration, the involvement of nerve compression, and other individual factors. If you are experiencing any of these symptoms, it is recommended to consult with a healthcare professional for an accurate diagnosis and appropriate management.
Differential Diagnosis
When evaluating symptoms related to the neck and cervical spine, healthcare professionals consider various conditions that can present with similar symptoms to cervical spondylosis. It’s important to differentiate between these conditions to provide appropriate treatment. Here are some common differential diagnoses to consider:
- Cervical Disc Herniation: This occurs when the gel-like center (nucleus pulposus) of an intervertebral disc protrudes or leaks out through a tear in the outer fibrous ring (annulus fibrosus). It can cause similar symptoms to cervical spondylosis, including neck pain, radiculopathy (radiating pain, numbness, or tingling in the arms), and muscle weakness. Imaging tests like MRI or CT scans can help in distinguishing between cervical disc herniation and cervical spondylosis.
- Cervical Spinal Stenosis: This condition involves the narrowing of the spinal canal in the cervical spine, leading to compression of the spinal cord or nerve roots. Symptoms may include neck pain, radiculopathy, muscle weakness, and balance problems. Differentiating between cervical spondylosis and cervical spinal stenosis may require imaging studies and a detailed evaluation of symptoms.
- Cervical Radiculopathy: Radiculopathy refers to the compression or irritation of a nerve root in the cervical spine. It can cause symptoms similar to cervical spondylosis, such as neck pain, radiating pain, numbness, tingling, or weakness in the shoulders, arms, and hands. Identifying the specific nerve root involved and correlating it with imaging findings can aid in distinguishing cervical radiculopathy from cervical spondylosis.
- Fibromyalgia: Fibromyalgia is a chronic condition characterized by widespread musculoskeletal pain, fatigue, and tenderness in specific tender points. Although it primarily affects muscles, it can also cause neck pain and stiffness, which may overlap with symptoms of cervical spondylosis. A thorough evaluation is needed to differentiate between the two conditions.
- Rheumatoid Arthritis: Rheumatoid arthritis is an autoimmune condition that primarily affects the joints, including those in the cervical spine. It can cause inflammation, pain, stiffness, and limited range of motion in the neck. Distinguishing rheumatoid arthritis from cervical spondylosis may involve a combination of medical history, physical examination, blood tests, and imaging studies.
- Myofascial Pain Syndrome: This condition involves the presence of trigger points or muscle knots that cause localized or referred pain and tenderness. Myofascial pain syndrome can cause neck pain and stiffness, similar to cervical spondylosis. A careful examination of trigger points and response to specific treatments can aid in differentiating between the two conditions.
These are just a few examples of conditions that can present with symptoms similar to cervical spondylosis. It is crucial to consult with a healthcare professional who can evaluate your specific symptoms, perform a thorough examination, and order appropriate tests to arrive at an accurate diagnosis and provide suitable treatment options.
Diagnosis:
The diagnosis of cervical spondylosis involves a comprehensive evaluation that includes a combination of medical history, physical examination, and imaging studies. Here are the key components of the diagnostic process:
- Medical History: The healthcare professional will begin by taking a detailed medical history, including a discussion of your symptoms, their duration, and any factors that worsen or alleviate them. They will also inquire about any previous injuries or conditions related to the neck or spine. Providing a thorough and accurate description of your symptoms is essential for an accurate diagnosis.
- Physical Examination: A physical examination will be performed to assess your neck mobility, strength, reflexes, and sensation. The healthcare professional may palpate the neck and spine to identify areas of tenderness or abnormality. They will also assess your posture, gait, and overall physical function. The physical examination can help evaluate the severity of your symptoms and determine if there are any specific neurological deficits.
- Imaging Studies: Imaging studies are commonly used to visualize the structures of the cervical spine and identify any abnormalities. These may include:
- X-rays: X-rays can provide a basic view of the cervical spine and help identify any degenerative changes, such as bone spurs or narrowing of the disc spaces.
- Magnetic Resonance Imaging (MRI): MRI uses powerful magnets and radio waves to generate detailed images of the cervical spine. It can show the condition of the discs, nerves, and soft tissues, making it useful for identifying herniated discs, spinal stenosis, or nerve compression.
- Computed Tomography (CT) Scan: CT scans can provide detailed cross-sectional images of the cervical spine, showing the bones, discs, and spinal canal. CT scans are particularly useful for assessing bony abnormalities, such as fractures or bone spurs.
- Electromyography (EMG) and Nerve Conduction Studies (NCS): In some cases, electromyography and nerve conduction studies may be recommended to evaluate the electrical activity and functioning of the nerves and muscles. These tests can help determine if there is nerve compression or damage and identify the specific nerves involved.
- Differential Diagnosis: As mentioned earlier, the healthcare professional will consider other conditions with similar symptoms and may perform additional tests or refer you to specialists as needed to rule out other potential causes.
It’s important to note that the diagnostic process can vary depending on individual circumstances and the severity of symptoms. Consulting with a healthcare professional, such as a primary care physician or a specialist like a neurologist or orthopedic surgeon, is crucial for an accurate diagnosis and appropriate management plan.
Treatment of Cervical Spondylosis
The treatment of cervical spondylosis aims to alleviate symptoms, improve function, and prevent further progression of the condition. The specific treatment options can vary based on the severity of symptoms, individual needs, and the healthcare professional’s recommendations. Here are some common approaches to managing cervical spondylosis:
- Non-Surgical Treatments:
- Physical Therapy Treatment: A physical therapist can provide exercises and techniques to improve neck mobility, strengthen supporting muscles, and enhance posture. They may also use modalities such as heat or cold therapy, ultrasound, or electrical stimulation for pain relief.
- Medications: Over-the-counter pain relievers such as nonsteroidal anti-inflammatory drugs (NSAIDs) may be recommended to alleviate pain and reduce inflammation. In some cases, stronger prescription medications or muscle relaxants may be prescribed for more severe pain or muscle spasms.
- Neck Braces/Collars: Soft neck collars or braces may be used for a short period to provide support, restrict movement, and alleviate pain. However, their long-term use is generally discouraged as it can weaken neck muscles.
- Lifestyle Modifications: Adopting healthy habits such as maintaining proper posture, avoiding prolonged sitting or repetitive neck movements, and engaging in regular exercise can help manage symptoms and prevent further deterioration.
- Pain Management Techniques: Additional pain management approaches may include hot or cold therapy, transcutaneous electrical nerve stimulation (TENS), acupuncture, or massage therapy.
- Surgical Interventions:
- Surgery is generally considered when non-surgical treatments fail to provide sufficient relief or when there is significant nerve compression or spinal cord dysfunction. The specific surgical procedure will depend on the underlying causes and severity of the condition. Common surgical interventions include:
- Discectomy: The removal of part or all of a herniated disc that is causing nerve compression.
- Spinal Fusion: Joining two or more vertebrae together to provide stability and reduce pain caused by abnormal motion.
- Artificial Disc Replacement: Replacement of a damaged or degenerated disc with an artificial disc to maintain spinal motion and alleviate pain.
- Surgery is generally considered when non-surgical treatments fail to provide sufficient relief or when there is significant nerve compression or spinal cord dysfunction. The specific surgical procedure will depend on the underlying causes and severity of the condition. Common surgical interventions include:
- Assistive Devices: In some cases, assistive devices such as a cervical collar or supportive pillows may be recommended to provide additional support and relieve strain on the neck during sleep or daily activities.
- Education and Self-Care: Educating oneself about cervical spondylosis, its management, and preventive measures is crucial. Practicing self-care, such as maintaining a healthy weight, avoiding smoking, practicing good posture, and engaging in regular exercise, can help manage symptoms and promote overall spine health.
The appropriate treatment plan for cervical spondylosis should be determined in consultation with a healthcare professional who can evaluate individual circumstances and recommend the most suitable options. They may refer you to specialists, such as physical therapists or pain management specialists, to provide targeted care and support throughout the treatment process.
Physical therapy Treatment
Physical therapy plays a crucial role in the treatment of cervical spondylosis. A physical therapist can design a personalized treatment plan to address specific symptoms, improve neck mobility, strengthen muscles, and promote overall function. Here are some common physical therapy interventions for cervical spondylosis:
- Neck Exercises: Physical therapists can prescribe specific exercises to improve neck mobility, flexibility, and strength. These exercises may include neck stretches, range-of-motion exercises, and strengthening exercises for the neck and upper back muscles. Examples of exercises include neck rotations, chin tucks, lateral neck stretches, and shoulder blade squeezes.
- Posture Correction: Correcting posture is an essential component of physical therapy for cervical spondylosis. Physical therapists can provide guidance on maintaining proper posture during daily activities, such as sitting, standing, and lifting. They may also recommend ergonomic modifications in the workplace or while using electronic devices to reduce strain on the neck.
- Manual Therapy: Manual therapy techniques performed by physical therapists can help relieve pain, improve neck mobility, and reduce muscle tension. These techniques may include gentle joint mobilizations, soft tissue mobilization, manual traction, or massage therapy targeted at the neck and upper back muscles.
- Heat or Cold Therapy: The application of heat or cold to the neck area can help reduce pain and inflammation. Physical therapists may use heat packs, cold packs, or alternate between both modalities to provide pain relief during therapy sessions.
- Electrical Stimulation: Transcutaneous electrical nerve stimulation (TENS) is a technique where low-level electrical currents are applied to the skin to reduce pain. TENS may be used by physical therapists as part of the treatment plan for cervical spondylosis.
- Education and Self-Management: Physical therapists provide education on cervical spondylosis, its causes, and strategies for self-management. They can teach proper body mechanics, exercises for self-care, and home-based stretching and strengthening routines to help individuals manage their symptoms and prevent recurrence.
- Modalities: Physical therapists may also use additional modalities such as ultrasound, laser therapy, or therapeutic ultrasound to provide pain relief, reduce inflammation, or promote tissue healing. These modalities are typically used in conjunction with other treatment approaches.
The frequency and duration of physical therapy sessions will vary depending on individual needs and the severity of symptoms. Regular communication with the physical therapist is important to track progress, modify the treatment plan as needed, and ensure proper adherence to the exercises and techniques prescribed.
It’s worth noting that physical therapy is just one aspect of a comprehensive treatment plan for cervical spondylosis. It is often combined with other non-surgical interventions, lifestyle modifications, and, in some cases, medical or surgical treatments. Consulting with a healthcare professional, such as a physical therapist or orthopedic specialist, is essential to receive appropriate guidance and care for your specific condition.
Exercise for Cervical Spondylosis
Exercise can play a beneficial role in managing cervical spondylosis by improving neck mobility, strengthening muscles, and reducing pain. However, it’s important to consult with a healthcare professional or a physical therapist before starting any exercise program to ensure that it is safe and appropriate for your specific condition. Here are some exercises commonly recommended for cervical spondylosis:
- Neck Range-of-Motion Exercises:
- Neck Rotations: Gently rotate your head from side to side, aiming to look over each shoulder without causing pain or discomfort.
- Neck Flexion and Extension: Slowly lower your chin towards your chest to stretch the back of your neck (flexion) and then lift your head upward, looking towards the ceiling (extension).
- Lateral Neck Bends: Tilt your ear towards your shoulder on each side, aiming to feel a gentle stretch on the opposite side of your neck.
- Neck Stretching Exercises:
- Levator Scapulae Stretch: Tilt your head to one side and slightly forward, then use your hand to gently pull your head downward towards your armpit until a stretch is felt in the side of your neck.
- Upper Trapezius Stretch: Tilt your head to one side and slightly forward, then use your hand to gently pull your head towards the opposite shoulder until a stretch is felt along the side of your neck and upper back.
- Chin Tucks: Sit or stand with good posture, then retract your chin back, creating a double chin. Hold the position for a few seconds and repeat.
- Strengthening Exercises:
- Scapular Retraction: Squeeze your shoulder blades together while keeping your neck and shoulders relaxed. Hold for a few seconds and release.
- Isometric Neck Exercises: Gently press your hand against your forehead, temple, or the back of your head, and resist the pressure with your neck muscles without actually moving your head. Hold each position for a few seconds and repeat in different directions.
- Shoulder Shrugs: Lift your shoulders up towards your ears, hold for a few seconds, and then relax. Repeat the motion several times.
- Posture Exercises:
- Shoulder Rolls: Roll your shoulders in a circular motion, first forward and then backward, to help improve posture and relieve tension in the neck and upper back.
- Chin Retractions: Sit or stand with good posture, then gently retract your chin back, creating a double chin. Hold the position for a few seconds and repeat.
It’s important to start these exercises slowly and gradually increase intensity and range of motion as tolerated. Be mindful of your body’s response and stop any exercise that causes pain or discomfort. Additionally, maintaining good posture throughout the day, taking breaks from prolonged sitting or computer use, and practicing relaxation techniques can further support the management of cervical spondylosis.
Remember, it is crucial to consult with a healthcare professional or physical therapist before starting any exercise program to ensure that it is appropriate for your specific condition and to receive personalized guidance based on your individual needs and limitations.
How to Prevent Cervical Spondylosis?
While it may not be possible to completely prevent cervical spondylosis, there are several measures you can take to reduce the risk of developing the condition or minimize its progression. Here are some preventive strategies:
- Maintain Good Posture: Practice proper posture while sitting, standing, and engaging in activities. Avoid slouching or hunching over, and make sure to keep your spine aligned. Use ergonomic chairs and equipment that provide adequate support for your neck and back.
- Take Regular Breaks: If you have a job or activity that involves prolonged sitting or repetitive neck movements, make it a habit to take regular breaks. Stand up, stretch, and change positions periodically to relieve stress on your neck and spine.
- Use Ergonomic Equipment: Ensure that your work environment is ergonomically designed. Adjust your desk, chair, and computer monitor to maintain a neutral and comfortable position for your neck and spine. Use a headset or speakerphone for extended phone conversations to avoid cradling the phone between your shoulder and ear.
- Practice Neck Exercises: Engage in regular neck exercises and stretches to improve neck flexibility, strengthen muscles, and maintain range of motion. Consult with a healthcare professional or physical therapist to learn proper techniques and exercises suitable for your condition.
- Exercise Regularly: Engage in regular physical activity to strengthen muscles, improve flexibility, and maintain overall spine health. Include exercises that promote good posture and strengthen the muscles of the neck, shoulders, and upper back.
- Maintain a Healthy Weight: Excess weight can put additional stress on your spine, including the cervical region. Maintain a healthy weight through a balanced diet and regular exercise to reduce the risk of developing cervical spondylosis or exacerbating existing symptoms.
- Avoid Repetitive Strain: Be mindful of activities that involve repetitive neck movements or strain, such as prolonged computer use or heavy lifting. Take breaks, vary your tasks, and use proper lifting techniques to minimize strain on your neck and spine.
- Use Proper Pillow and Mattress: Choose a pillow and mattress that provide adequate support for your neck and spine. The right pillow should help maintain proper alignment while sleeping and minimize strain on the neck.
- Quit Smoking: Smoking can contribute to the degeneration of spinal discs and impair blood flow, affecting the health of your spine. Quitting smoking can improve your overall spine health and reduce the risk of developing cervical spondylosis.
- Regular Check-ups: Schedule regular check-ups with your healthcare professional to monitor your spinal health and address any concerns or symptoms promptly.
It’s important to note that while these preventive measures can help reduce the risk and progression of cervical spondylosis, they may not guarantee complete prevention. If you experience any persistent neck pain, stiffness, or other concerning symptoms, it’s essential to seek medical attention for proper evaluation and management.
Conclusion
Cervical spondylosis is a degenerative condition that affects the cervical spine (neck region). It is characterized by the wear and tear of the spinal discs, bones, and joints in the neck. Here is a summary of key points about cervical spondylosis:
- Cervical spondylosis is caused by age-related changes in the cervical spine, such as disc degeneration, bone spurs, and ligament thickening.
- Common symptoms include neck pain, stiffness, headaches, radiating pain or numbness in the arms or shoulders, muscle weakness, and decreased range of motion.
- Differential diagnosis is important to rule out other conditions that can cause similar symptoms, such as herniated discs, spinal stenosis, or nerve impingement.
- Diagnosis involves a combination of medical history, physical examination, and imaging studies like X-rays, MRI, or CT scans.
- Treatment options include non-surgical approaches like physical therapy, medication, lifestyle modifications, and pain management techniques. In severe cases, surgery may be necessary.
- Physical therapy plays a significant role in managing cervical spondylosis by providing exercises to improve neck mobility, strengthen muscles, and promote good posture.
- Preventive measures include maintaining good posture, taking regular breaks from prolonged sitting, using ergonomic equipment, practicing neck exercises, regular exercise, maintaining a healthy weight, avoiding repetitive strain, using proper pillows and mattresses, quitting smoking, and scheduling regular check-ups with healthcare professionals.
It’s important to consult with a healthcare professional, such as a primary care physician, orthopedic specialist, or physical therapist, for an accurate diagnosis and personalized treatment plan based on individual needs.